


An external report costing £64,000 has revealed further issues within Jersey's radiology and orthopaedic departments – including concerns that the software on the current MRI scanner is so out-of-date that it is not possible to screen for prostate cancer.
The report also revealed that the Government paid out £600,000 between 2021 and 2023 for orthopaedic litigation claims for public patients.
Announcing the report's publication to the media, Health Minister Tom Binet said: "In the past, a report of this nature would not normally be released.
"However, having discussed with senior officers, we are all of the opinion that it would be helpful for you to have sight of the work that is being undertaken to ensure the best long-term use of public funds."
The report was authored by Professor Tim Briggs, Graham Lomax, Dan Pearce from Getting It Right First Time (GIRFT), a UK programme that focuses on improving the quality of care within healthcare settings by reducing unnecessary variations.
Whilst GIRFT reviews all specialities of surgery and medicine, the review of the Jersey General Hospital was undertaken to explore opportunities to improve both orthopaedic services and theatre efficiency.
In the introduction to the report, Prof Briggs – Chair of GIRFT and NHS England National Director for Clinical Improvement and Elective Recovery – said that Hospital staff "were very open and honest in providing views on where they felt there were challenges and recognised that there is a real opportunity to improve services".
"We saw excellent facilities, with many examples of good practice," he wrote.
"This confirms our view that Jersey General Hospital has an opportunity to become an exemplar hospital, which will improve care for all patients and encourage additional private patients to use the facilities."
A total of 36 recommendations were outlined by the reviewers, who visited the Hospital for two days in April 2024.
The report recommended that the Health Department should undertake a review of current radiology equipment and upgrade where necessary.
“We were told that the equipment is old and the software on MRI scanner requires updating as currently it is not possible to screen for prostate cancer," said reviewers.
It comes after a recent Royal College of Physicians review of radiology found that "aggression" and "gatekeeping" had destroyed diagnosis opportunities.
As a result, 20 women had to be recalled for a breast cancer screening over fears of a possible misdiagnosis by a radiologist, while a further 14 were told that their diagnosis was initially missed – in some cases delaying their treatment for up to a year.

Pictured: Reviewers were told that the software on the Hospital's MRI scanner requires updating as currently it is not possible to screen for prostate cancer.
The GIRFT report also flagged the fact that the out-of-hours radiology provision relies on staff volunteering to cover the service, and raised concerns that there is no access to a 24/7 MRI imaging service for patients with suspected Cauda Equina Syndrome (CES).
The report explained that CES is a spinal surgical emergency which can lead to lower limb paralysis and loss of bowel, bladder and sexual function if not assessed and treated urgently.
More than 20% of litigation claims for spinal surgery in England relate to CES, according to GIRFT.
The report explained: "When acute CES is suspected, timely diagnosis is crucial, and there should be access to a 24/7 MRI imaging service in these cases."
Reviewers recommended that the skills of local radiographers should be expanded to allow out-of-hours MRIs for patients presenting with suspected CES.
The report suggested that this recommendation should be completed within three to six months.
"Once a MRI for suspected CES has been performed it can be sent digitally to Southampton for their opinion," the review recommended.
Pictured: The report raised concerns that approximately 65% of the radiology team are employed under a locum contract.
The report also criticised the high number of locum staff within the Radiology Department, with approximately 65% of the team employed under a locum contract.
Reviewers recommended that Health should undertake a workforce review to determine the number of staff required to provide an efficient service.
"Further work needs to be done to reduce long term locums and to make substantive posts more attractive to staff," the report said.
The report revealed that the Government paid out £600,000 between 2021 and 2023 for orthopaedic litigation claims for public patients.
Reviewers recommended that the Hospital should undertake an annual review of litigation claims in detail – including expert witness statements, panel firm reports and counsel advice as well as medical records – to determine where patient care or documentation could be improved.
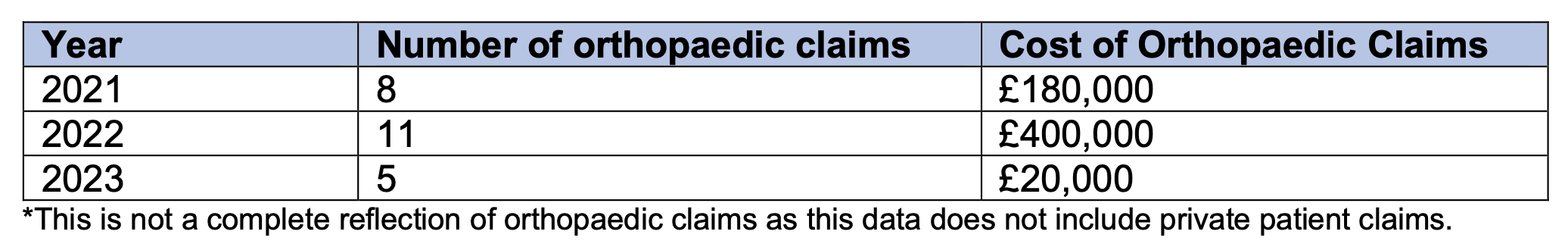
Pictured: The table shows the number of orthopaedic litigation claims and the costs associated with the claims for publicly-funded patients.
Within the Orthopaedic Department, concerns were raised about the high usage of uncemented hip fixations being used in patients over the age of 65.
"At least 80% of patients over 70 years of age should be receiving a fully cemented or hybrid hip replacement," the report said.
Reviewers also identified a high 'return to theatre' rate for primary hip surgeries.
The report recommended that Health should "undertake review of all orthopaedic readmission surgery data to identify themes, understand outcomes and establish an improvement strategy", and audit it on an annual basis.
Reviewers also identified that patients over the age of 75 who were undergoing emergency repairs for neck fractures were staying in hospital for longer than necessary.
"We were told that there are delays with discharging the trauma patients because the community package of care is not available," they said.

Pictured: Reviewers raised concerns that "several surgeons" were doing five procedures or less per year – which is associated with increased complications.
When reviewing the number of orthopaedic procedures carried out by each surgeon, reviewers raised concerns that "several surgeons" were doing five procedures or less per year.
"Surgeons delivering less than 10 hip and knee revisions over three years should no longer be performing this surgery," the report said.
"Operations delivered by surgeons who perform a very low volume of that surgery type are associated with increased lengths of stay, complications and cost."
The reviewers also told that the surgical lists of middle grade doctors had been reduced or reallocated and given to consultants who would perform the surgical tasks more quickly.
"This has had a negative impact on staff morale and has deskilled middle grade doctors and increased the risk of them leaving Jersey for other opportunities," the report said.
"We felt that if this happened, recruitment to these vacant posts would be difficult."
Many other recommendations throughout the review also focussed on staffing concerns – including the high number of locums, agency staff and interims.
The report recommended that the Health Department should make substantive posts more attractive to staff, as well as considering applicants from oversees.
Concerns were also raised about the fact that physiotherapists and occupational therapists are on civil service contracts, which limits their ability to provide weekend cover.

Pictured: The report raised concerns about the fact that physiotherapists and occupational therapists are on civil service contracts, which limits their ability to provide essential weekend cover.
The reviewers found that the current system of weekend working relies on the good-will of staff volunteers which was criticised as being unsustainable and not cost effective.
They recommended that Health "carry out a review of employment contracts and remove any limitations to allow weekend and out of hours working".
Other staffing recommendations focussed on upskilling employees and tackling high absences rates.
The report also urged "rapid engagement of the clinical and operational workforce around the new hospital strategy", deeming this as "critical in terms of planning and delivering a successful transition".
Other recommendations focussed on how the Hospital could best utilise surgical theatres to optimise usage through, for example, appropriate scheduling and upskilling staff.
The report recommended that certain surgical procedures should be performed in an outpatient procedure room by default, not inpatient theatres, to bring the Hospital in line with GIRFT’s ‘right procedure, right place’ approach.
Opportunities to increase the number of cases performed per theatre session were also identified, including day case pathways and job planning for staff across the whole of the week to maintain activity across five or six days.
"We found that the staff are willing and excited about the challenges to use the data they have, to effectively identify variation and drive change to improve services," said Prof Briggs.
The report also recommended that Health should establish a pool of standby patients to fill gaps in theatre schedules promptly, especially when there are cancellations or unexpected openings.
"This will optimise theatre capacity and ensure efficient use of resources," the report said.
Elsewhere in the report, reviewers also raised concerns about the fact that the Sterile Services Department – which is responsible for cleaning the medical devices and equipment used in surgery – is located offsite near Five Oaks.
"We were told that this creates a problem with tray turnaround which then has an impact on the time it takes to process trays that have bodily fluids dried on them," they said.

Pictured: The Sterile Services Department is responsible for cleaning the medical devices and equipment used in surgery.
The report found that there are delays with delivering and collecting equipment as the drivers often have to wait in a queue at the hospital delivery point, resulting in delays of up to 45 minutes.
Reviewers recommended that the number of deliveries should be increased to six times a day, and Health should give ‘blue light priority’ to drivers at the delivery point.
It also emerged that that Sterile Services Department "requires two additional washers and one additional steriliser to provide an efficient service".
Reviewers described it as "essential" that space is identified for this new equipment at both the Hospital and Sterile Services Department site.
The full Getting It Right First Time (GIRFT) can be read online.
INSIGHT: How "aggression" and "gatekeeping" destroyed diagnosis opportunities
Neurology next for independent review amid “ongoing issues and concerns”
FOCUS: “You need to accept you have a problem”
Health could face lawsuit over radiology misdiagnosis fears
Panel "should have been made aware" of radiology scandal
Tip of the iceberg? “Other issues” in radiology under investigation
MRI scanner left out of action after routine service
IN-DEPTH: “How much evidence does Jersey's health department need?"
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.