

A new report has uncovered "systemic gender inequalities" putting women and girls in Jersey at "a greater risk of poor health" – but what is driving this trend? And what can be done to address it?
The island's first-ever Women's Health and Wellbeing Assessment, which was launched by the Health Minister two years ago, aimed to identify key challenges faced by the female population, understand the contributing factors, and provide a "robust evidence base" to inform policies and interventions to support women's health in future.
Based on extensive research including over 1,650 survey responses and professional consultations, the assessment aimed to promote a whole-system view – looking not just at health services but also the wider factors affecting the health of women and girls.
The result is a 59-page document that uncovers "systemic gender inequalities" touching every aspect of women's lives – from access to healthcare and education to the lingering effects of gender-based violence.

Pictured: The 59-page document uncovers "systemic gender inequalities" touching every aspect of women's lives.
Women earn lower wages than men, experience higher levels of financial stress and insecurity, face greater mental health challenges, deal with economic pressures related to the high cost of childcare, and suffer from the mental strain of balancing work and family responsibilities.
These challenges have long-term impacts on women’s health, according to the report, and lead to poorer outcomes and lower life quality.
It concludes, therefore, that women and girls are at a greater risk of poor health than men, and these risks are driven by a combination of biological, social, and economic factors.
The report said: "In 2024, women and girls continue to face systemic gender inequalities. By the very nature of being a woman or girl, they are at a greater risk of poor health."
But what exactly are the findings...
Although women are living longer, they are spending more of those years in poor health compared to their male counterparts.
The data shows that on average, females in Jersey can expect to spend around 24 years of their life in poor health, compared to only 18 years for men.
Alcohol consumption among women in Jersey surpasses levels seen in England, particularly among the 45–54 age group, while poor diet, obesity, and low physical activity remain prevalent among lower-income women.
One-in-two women and one-in-three girls are classified as overweight or obese, and only 5% of teenage girls meet daily physical activity recommendations.
Only 27% of women feel their mental health needs are being adequately met, while one-in-four experience loneliness frequently.
Teenage girls are particularly affected, with rising rates of mental health issues linked to financial stress, social isolation, and a lack of trauma-informed care.
The report suggests that many women who experience violence or trauma are left without adequate support.
Nearly half of teenage girls reported experiencing inappropriate sexual attention or comments, while violence against women and girls remains a leading cause of homelessness among women.
The report notes that dismissive and misogynistic attitudes towards women's health issues lead to the stigmatisation of women's health problems, which can be a barrier to accessing care.
Attitudes toward reproductive and gynaecological health are identified as a persistent issue in the report.

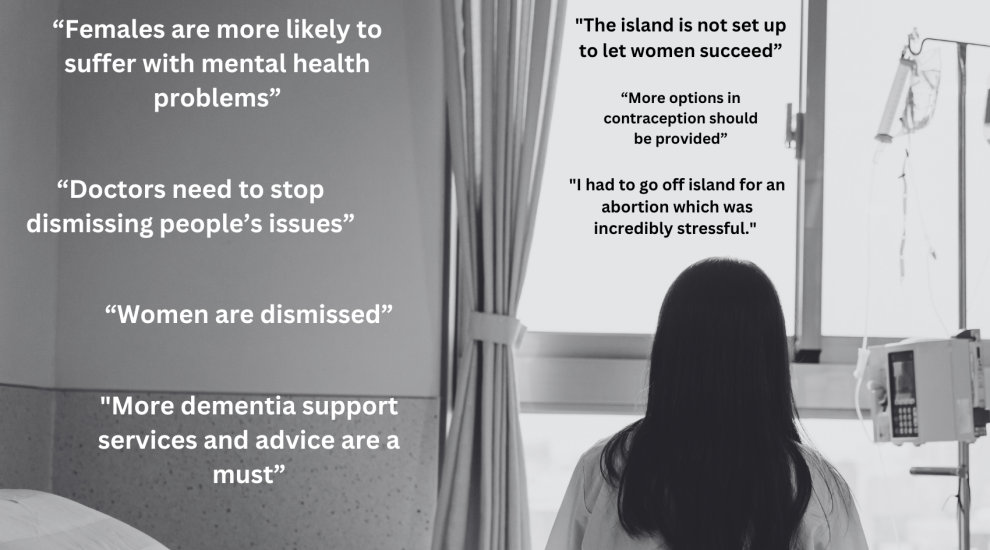
Pictured: Survey respondents raised concerns about “medical misogyny” in Jersey.
Survey respondents felt that topics such as menstruation, miscarriage, and menopause are still stigmatised, leaving many women without the care and support they need.
One woman called on policymakers to "address medical misogyny in all levels of the health service".
Another respondent added: “Doctors need to stop dismissing people’s issues and actually look into concerns.
"Help with symptom management and continue to test if you can’t figure out what’s wrong."
But healthcare is not the only area in which sexist beliefs impact the wellbeing of women, as one stakeholder explained.
"Unchecked and ongoing misogyny and sexism within structures such as education, health and criminal justice," they said.
"Outdated laws that favour males financially. Discrepancies in pay within employment. All of these inequalities place an additional stress burden on women and girls, navigating systems that are less accessible to them."
The report also points to socioeconomic challenges, particularly for women in lower-income brackets.
Women in Jersey are disproportionately affected by financial stress – with the public sector pay gap rising from 18.3% in 2018 to 24.3% in 2020.
Pictured: Women in Jersey are disproportionately affected by financial stress.
Single mothers, who make up 88% of single parents, are particularly vulnerable to economic pressures. The high cost of childcare, 37% higher than in England, makes it difficult for many women to balance work and family responsibilities.
This financial strain also limits access to quality healthcare, healthy food, and adequate housing – all of which have direct impacts on women’s overall health.
"The island is not set up to let women succeed; we are always expected to compromise on something,” one woman was quoted saying in the report.
"When you work two jobs to meet basic needs, it’s a real struggle to find the additional money needed for healthcare,” another added.
In summary, the combination of biological factors, societal attitudes, and socioeconomic challenges contribute to women in Jersey experiencing poorer health outcomes and spending more of their lives in poor health compared to men.
And while the report does not provide recommendations – and instead focuses on presenting a robust evidence base that can be used by decision-makers in government and the community – it does make a case for change.
It calls for investment in preventative health measures, improvements in mental health support, addressing wider social determinants affecting women's health, and reducing barriers to healthcare access.
To prevent diseases, they called on policymakers to invest in healthy behaviours from childhood, including reducing alcohol consumption, promoting healthy eating, increasing physical activity, and fostering better sleep and social connections.

Pictured: The report calls for normalising conversations around topics such as menstruation, miscarriage, and menopause.
To improve gynecological and reproductive health, the report calls for normalising conversations around menstruation, miscarriage, and menopause while addressing dismissive attitudes in the provision of specialise face.
The report also suggested improving mental health support by providing targeted mental health services during key life stages, including adolescence, the perinatal period, and post-trauma recovery.
To address wider issues, the report suggested tackling systemic challenges such as financial strain, housing costs, childcare expenses, and gender-based pay gaps that impact women's ability to prioritize health.
It also called on policymakers to address the health and workforce challenges posed by declining birth rates and Jersey's ageing population, while ensuring women play a central role in the island's future economic growth.
The Director of Public Health welcomed the findings, calling them a “rich evidence base” that decision-makers can use to address inequalities and improve outcomes for women and girls.
Professor Peter Bradley said: "Many of the findings of this report do not come as a surprise but show that the island has some significant issues, and the health of our population is impacted by a range of determinants, most outside of the control of individuals."
He explained these findings come as the healthcare system undergoes significant changes, including the formation of Jersey Health and Care and the establishment of a new Partnership Board to improve collaboration across the health system.

Pictured: The transition to a new "stand-alone" health department is set to begin in Jersey next year.
The Women’s Health and Well-being Joint Strategic Needs Assessment was published on 18 December by the Public Health Department, and forms part of Jersey's population health prevention strategy.
Detailed appendices will be published in January 2024 to offer a deeper dive into consultation responses, professional engagement insights, and service mapping.
Follow Express for updates...
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.