


Amid the recent turmoil plaguing Jersey's Health department, there is one topic which continuously seems to be at the centre of the conversation: should the island follow UK clinical guidelines, or should we be allowed to 'make up our own rules'?
The UK clinical guidance most often referenced during such discussions are the National Institute for Health and Care Excellence (NICE) guidelines.
NICE guidelines were introduced in 1999 to provide "evidence-based guidance" for health practitioners across the UK.
The guidance was first established in an attempt to end the so-called postcode lottery of healthcare in England and Wales, where availability and quality of treatment depended on the NHS Health Authority area in which the patient happened to live.
However, NICE has since acquired a high reputation internationally as a role model for the development of clinical guidelines.
Its aims are to help practitioners deliver the best possible care; give people the most effective treatments based on the latest evidence; provide value for money; and reduce inequalities and variation in healthcare across the country.
While Jersey is not covered formally by NICE, the organisation's guidelines are cited regularly as a benchmark for good care.
There is no alternative local policy in the island.
Whilst the recent rheumatology review is the most high profile example of Jersey not conforming to NICE guidelines, it is not the first time concerns have been raised.
In a critical report published in 2021, Jersey's maternity facilities were found to be “inadequate and highly unacceptable”.
Among the 48 findings and 29 recommendations laid out in the report were concerns that maternity policies were open to interpretation and were applied differently according to the specific member of staff, leading to a “discordance in care”.
The reviewers recommended that critical indicators need to be identified and agreed to allow the maternity team to determine whether the service is of high quality.
The report found that staff were presented with differing guidelines from different sources, including NICE, that sometimes conflicted with one another "causing confusion and an inconsistently in the approach taken".
It continued: "According to our advisers, it is unclear how often modification of policies/guidelines is necessary for Jersey specific issues and what this means in terms of safety of care."
The report suggested that "it may be most prudent to propose that all NICE guidelines are adopted unless there is an exception".
In an accompanying report from Attain Health Management, the largest independent health advisory and delivery organisation in the UK, advisors acknowledged that many policies based on NICE and other established guidelines – but noted that "there is no automatic process to adopt these guidelines for Jersey".
Whilst translation UK policies into Jersey policies was described as "time consuming", the report agreed that "for the majority of policies a simple process could be established allowing endorsement of a wider policy quickly, with only a few policies requiring substantive change".
The case which has sparked the most serious concerns about Jersey's relationship with UK clinical guidance was the recent review of the island's rheumatology department.
Published at the start of 2024, the Royal College of Physicians' report "found the standard of care to be well below what the review team would consider acceptable for a contemporary rheumatological service".
The report revealed a "lack of governance, not just in rheumatology but across the healthcare organisation".
At the centre of the report were concerns about the department's relationship with medical guidelines, noting that in some cases there was “no evidence of clinical examination” and there was “on occasions, an incorrect diagnosis”.
The review team heard from several interviewees about the reluctance to follow national or international guidance – such as National Institute for Health and Care Excellence or European League Against Rheumatism guidelines – as it "did not apply" in Jersey.
The review team was "concerned" to learn that alternative local policies to these guidelines did not exist in the island.
The report said: "Worryingly, an individual approach was taken whereby consultants were allowed to do their own research and make their own decisions on which medications they chose to provide to patients without a secondary review by the pharmacy team."
Concerns were also raised about the lack of requirement for prescriptions to include the clinical indications for treatment, and prescriptions would not be checked for clinical indications for treatments or blood monitoring results.
The review found that medication doses would not be checked for compliance with national guidance by the pharmacy team "as they reportedly did not have the staffing capacity and access to the clinical records".
A recent audit of medicinal cannabis prescriptions in the island revealed a "significant" difference in prescribing levels between Jersey and England – with 6% of the island's working population holding a prescription compared to just 0.05% over the water.
The Government said that the audit also found evidence that some patients had been receiving prescriptions from two or more prescribers in the same month.
And some of those were for amounts that "could reasonably be assumed to be for more than one month's supply" – something highlighted as being in breach of NHS and NICE guidelines.
The results of the audit sparked alarm in Government, and work to develop the policy that will inform the legislative framework to regulate and inspect cannabis clinics commenced shortly after.
However, new legislation is not likely to be ready for debate in the States Assembly until 2026.
In public meetings of the Health Advisory Board, experts have been emphatic about their desire to ensure the Health department is adhering to NICE guidance.
In monthly minutes dating back to October 2023, there are few documents that don't mention NICE guidelines as least once.
In December 2023, the Board urged the Health department to recognise that all processes to drive quality and safety must be followed – including NICE guidance.
The minutes noted: "The first step is to make sure the policies are in place, which HCS is doing currently, and the second (more difficult) step is ensuring compliance."
In the January 2024 minutes, the Board highlighted a report which showed that the Royal College of Physicians recommended a review of rheumatology consultant adherence to NICE guidelines back in 2016.
"However, this was not done as consultants did not want this," the board minutes read. "Therefore, this is a system issue."
During the same meeting, Health Chief Officer Chris Bown stated that the culture of good clinical governance is behind where you would expect to see it and work is required with clinicians to improve this, particularly in relation to following guidelines.
He noted that if appropriate guidelines were followed in the past, the rheumatology service would not have been in the position it was in January 2022.
The minutes state: "The Board has made clear it’s expectations regarding following NICE guidelines however, work is still required with clinicians led by the appropriate executives and Chiefs of Service.
"The Board will bring the momentum required to ensure that such are addressed, particularly the culture of good clinical governance."
In its February meeting, the Board confirmed that it had received assurance that the Health department had communicated the policy change to adhere with clinical guidelines.
"However, there is limited assurance that NICE [or] other evidence-based practice is being followed," the minutes said.
"Once recruited, this will be a priority for the Head of Compliance and Regulation as HCS prepares for inspection and is an important piece of work for the Medical Director and Chief Nurse to focus on.
"The committee will continue to monitor, noting that this will be a two-year plan. Escalations and exemptions will be reported to Board through this committee."
One of the key aims of the Health department's 'BeOurBest' programme includes the "adoption and implementation of NICE guidelines".
But despite this clear encouragement from Health experts, Jersey's politicians actually voted against aligning new IVF funding guidelines with NICE guidance in May this year.
Deputy Lucy Stephenson lodged a proposal in early April to reform existing funding for IVF, arguing that the current arrangement was "outdated".
Her proposition stipulated that any new funding model should reflect NICE clinical guidance on IVF – which currently recommend funding three full cycles of IVF for women under 40, or one full cycle for those aged between 40 and 42.
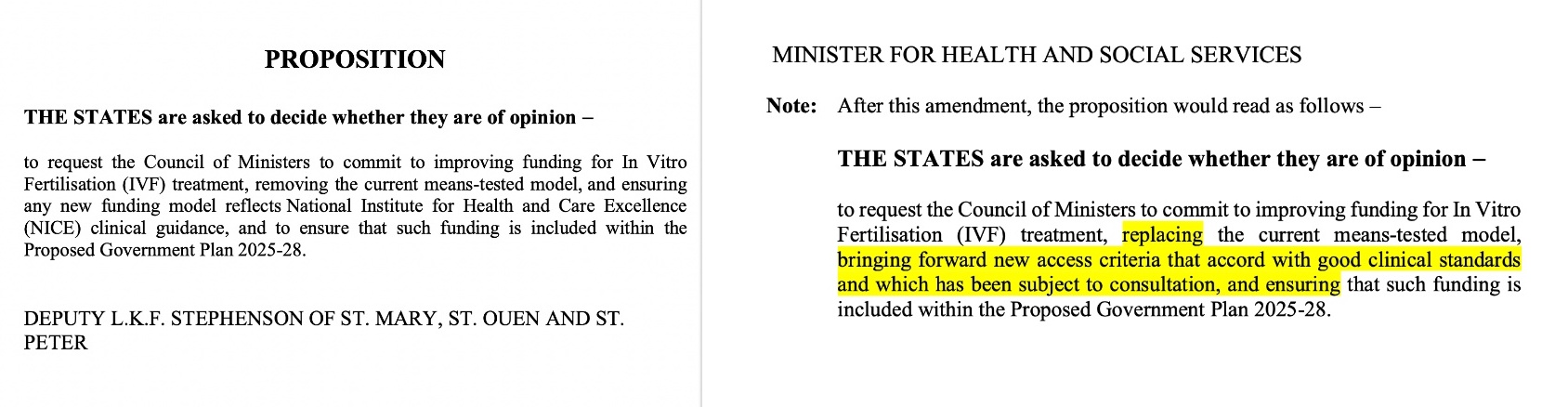
Pictured: Deputy Stephenson's proposition (left) compared to Deputy Binet's amendment (right).
However, Health Minister Tom Binet lodged an amendment to the proposition which said that new criteria related to financial support for IVF treatment should be developed in consultation before any changes to the funding model are made.
He said: "In so doing, we will ensure that any IVF service funded by the Government accords with good clinical standards – even if it does not provide up to three publicly funded IVF cycles for all people."
Ahead of the debate, Deputy Stephenson: "I am concerned that the Minister's amendment seeks to remove the clinical, evidence-based guidance from NICE from my proposition.
"This is especially disappointing given that in October the Health Advisory Board heard that the senior leadership team at Health and Community Services had agreed to adopt NICE guidance as the default position for clinical guidelines.”
This put the question of whether to follow NICE guidelines or not at the centre of the political debate.
In the States Assembly, Deputy Stephenson asked why the Government wanted to "create more work for itself" by creating its own guidance.
“It does feel like we are trying to re-invent the wheel and I question why,” she said.
Deputy Hilary Jeune agreed, stating that it was unclear how the island would develop its own “good clinical standards” given the recent performance of the department that has not been “up to scratch”.
Deputy Miles pointed to recent critical reports on local clinical standards, specifically in the maternity and rheumatology departments, which identified that prescribing in Jersey was outside any of the national and international guidance available, including NICE.
She argued Jersey should adopt NICE's “national best practice".
But Chief Minister Lyndon Farnham said: “We don’t want to become another NHS and we want to be able to choose and create our own rules that are right for Jersey.
"That is all that is behind the amendment.”
States Members ultimately backed the amendment lodged by Health Minister Tom Binet by 28 to 15 – which did not specify any compliance with NICE guidelines.
Following the debate, Deputy Stephenson warned that this was a "mistake".
In a States sitting just three weeks later, the Health Minister said that a "great deal of effort" has been expended by the Health department in trying to improve clinical standards and governance.
He was answering a question from Deputy Jonathan Renouf which asked: "Will the Minister provide an update on any plans he has to improve clinical standards and governance in the delivery of Health services?"
Deputy Binet replied: "In June last year, [the Health department] implemented a policy that mandated staff to follow NICE guidelines and Royal College guidance."
The Health Minister added that he would not be adding any further requirements to "this already substantial body of work".
"Given all of the other pressures involved in catching up with a long period of underinvestment and a leadership that has not kept pace, I did not think that would be helpful," he said.
"What I am trying to do is to ensure that the organisation is properly resourced and that it is provided with as much support as possible to implement the objectives that are already in hand."
In the same States sitting during a discussion about whether Jersey would follow the UK if it adopts an expert suggestion to make the chickenpox vaccine a routine childhood jab, the Health Minister said: "As for all such vaccination programmes, we look to the Joint Committee as our principal source of information for decision-making.
"As soon as the final recommendation is received from the UK Department of Health and Social Care, the matter will be discussed by Jersey and the decision will be made at that time."
In response, Deputy Lucy Stephenson quipped: "Can the Minister confirm why we look to the JCVI [Joint Committee on Vaccination and Immunisation] on such matters?
"Is it because they're experts in their field, and they've had the opportunity to undertake detailed research and assessments before making their recommendations – rather like NICE does?"
Deputy Binet replied: "I am led to believe that that is the case."
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.